About Eating Disorders
What Is an Eating Disorder?
Medical And Psychiatric Condition
An eating disorder (ED) is a medical and psychiatric condition that consists of disordered eating patterns that cause significant psychological distress and leads to impairment in an individual’s life in areas such as personal relationships, academics, work, and/or social interactions. However, an eating disorder can also be thought of as a dysfunctional coping mechanism such as alcohol and substance abuse.
While many individuals with an eating disorder may seem resistant to changing their behaviors, they usually wish they never had the ED to begin with. Often, the general public and misinformed individuals believe that an ED is about one’s preoccupation with wanting to “look good” and a desire to be thin. This is akin to saying an alcoholic drinks because he is thirsty. An eating disorder numbs and preoccupies an individual’s thoughts to the point where there is an “escape” from reality.

Behaviors And Physical Attributes
As a result, patients often lose connections with friends and family and suffer setbacks in work and academics. Furthermore, outsiders can only see a fraction of the behaviors and physical attributes of an eating disorder and never can see or experience what is going on inside the mind of a person suffering from it.
It is this mental dialogue that causes the great distress that truly defines an eating disorder. It is an internal voice that is constantly thinking and worrying about food, weight, body image, calories, exercise, and related eating disorder obsessions.
Additionally, that internal voice is very self-demeaning, telling oneself that they are a bad person, undeserving, and not worth anything. It is this component of the eating disorder that others are unaware of in a person who struggles, yet it is this component that makes ED so devastating.
Emotional Aspect Of Stressors
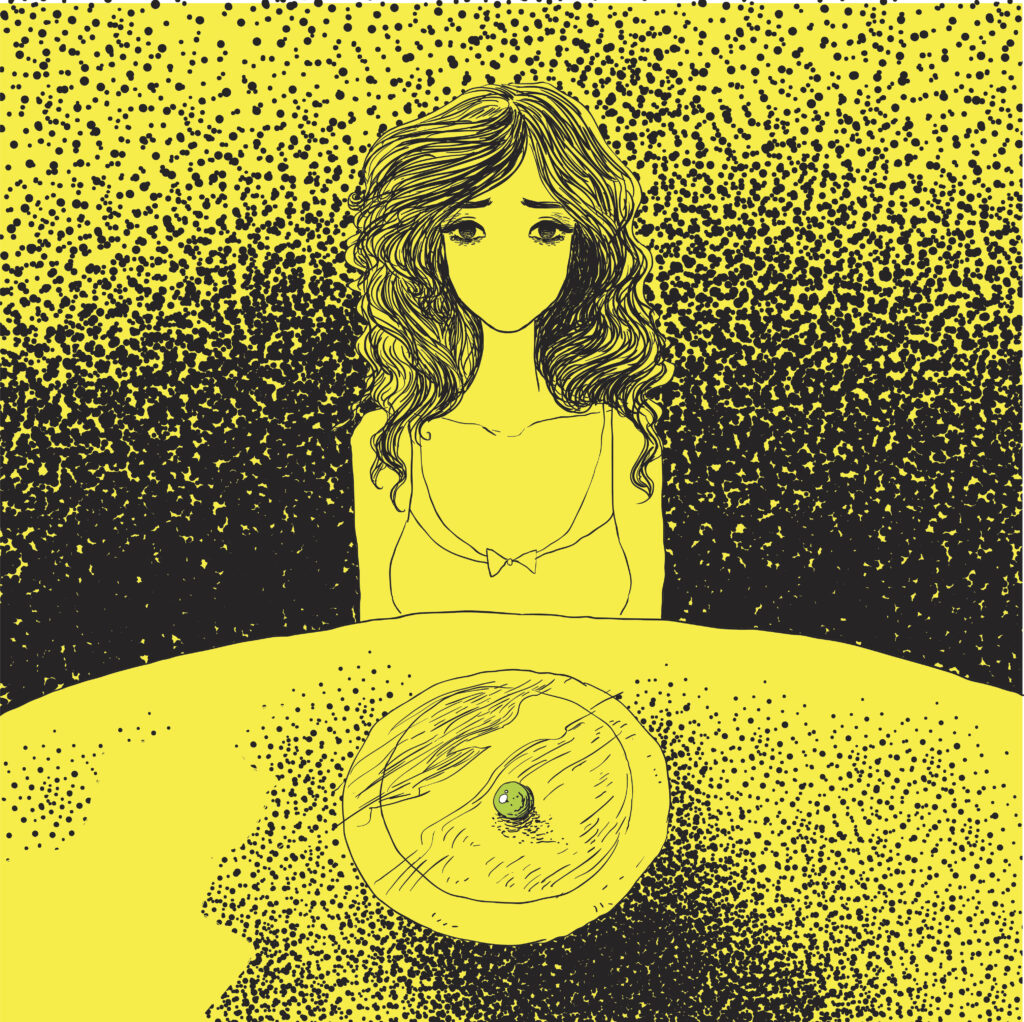
An eating disorder takes the intangible emotional world that at times can make someone feel they have no control over, and refocuses their thoughts on more tangible things. One cannot pick up and hold emotions. You cannot visually see emotions and they cannot be avoided. There are no numbers or units associated with emotions, so one cannot measure them.
People often feel they cannot control what emotions “come in” and what emotions “go out.” The emotional aspect of stressors in life can often not be avoided. But with an ED, one can look at foods, hold them, and see them. They can measure their calories or their weight and attempt to regulate those numbers.
They can decide what food goes in, and even what comes out. They can avoid certain foods, events, picnics, and restaurants. There is no need to, nor the time to, focus on the stressors in life that can create pressure.

Escape From Dealing With Life Stressors
An ED alters how a person feels. They do not feel sad, they “feel fat.” A false perception is formed that happiness can be achieved by reaching their eating disorder goals. Frustration occurs because there is no true happiness when a goal is reached. And the cycle continues.
Still, an eating disorder, despite its harmful and even potentially lethal effects, serves a purpose: it acts as a coping tool. Granted, not a healthy one, but nonetheless, to the individual, it is an escape from dealing with life stressors that cause pain to a person’s ego. An ED is a way to “self-medicate” just as alcohol, illicit drug use, gambling, sex, shopping addictions, and other harmful behaviors are for others.
The “side effects” of self-medicating with eating disorders are what makes them have the highest mortality rate (even greater than depression, bipolar disorder, schizophrenia, etc.) in all of psychiatry.
Diagnosing an Eating Disorder
For clinicians, the “official” diagnosis of an eating disorder is made by using the criteria listed in the Diagnostic and Statistical Manual V Edition (DSM-V).
DSM-V Diagnostic Criteria for Eating Disorders
Anorexia Nervosa
Anorexia nervosa (AN) is a disorder in which individuals exhibit significant weight loss and extreme restrictions in their food intake. It is estimated that 1%-2.2% of the population meet the criteria for this disorder, which includes:
- Restriction of energy intake relative to requirements, leading to significantly low body weight in the context of age, sex, developmental trajectory, and physical health. Significantly low weight is defined as a weight that is less than minimally normal or, for children and adolescents, less than minimally expected.
- Intense fear of gaining weight or of becoming fat, or persistent behavior that interferes with weight gain, even though at a significantly low weight.
- Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or persistent lack of recognition of the seriousness of the current low body weight.
Specify Whether:
Restricting type: During the last three months, the individual has not engaged in recurrent episodes of binge eating or purging behavior (i.e. self-induced vomiting, or the misuse of laxatives, diuretics, or enemas). This subtype describes presentations in which weight loss is accomplished primarily through dieting, fasting, and/or excessive exercise.
Binge-eating/purging type: During the last three months the individual has engaged in recurrent episodes of binge eating or purging behavior (i.e. self-induced vomiting, or the misuse of laxatives, diuretics, or enemas).

Bulimia Nervosa
Bulimia nervosa (BN) is a disorder in which individuals eat excessive amounts of food in a short period of time and, afterward, eliminate this food from their body through some type of purging behavior. It is estimated that between 1.1% to 4.2% of the female population suffers from BN. Criteria include:
A. Recurrent episodes of binge eating. An episode of binge eating is characterized by both:
- Eating in a discrete period of time (e.g. within any 2-hour period) an amount of food that is definitely larger than what most individuals would eat in a similar period under similar circumstances;
- A sense of lack of control over eating during the episodes (e.g. a feeling that one cannot stop eating or control what or how much one is eating.)
B. Recurrent inappropriate compensatory behaviors to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise.
C. The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for 3 months.
D. Self-evaluation is unduly influenced by body shape and weight.
E. The disturbance does not occur exclusively during episodes of anorexia nervosa.
Binge-Eating Disorder
A. Recurrent episodes of binge eating. An episode of binge eating is characterized by both:
- Eating in a discrete period of time (e.g. within any 2-hour period) an amount of food that is definitely larger than what most individuals would eat in a similar period under similar circumstances;
- A sense of lack of control over eating during the episodes (e.g. a feeling that one cannot stop eating or control what or how much one is eating).
B. Binge eating episodes are associated with three or more of the following:
- Eating much more rapidly than normal.
- Eating until feeling uncomfortably full.
- Eating large amounts of food when not feeling physically hungry.
- Eating alone because of feeling embarrassed by how much one is eating.
- Feeling disgusted with oneself, depressed, or very guilty afterward.
C. Marked distress regarding binge eating is present.
D. Binge eating occurs, on average, at least once a week for 3 months.
E. Binge eating is not associated with the recurrent use of inappropriate compensatory behavior as in bulimia nervosa and does not occur exclusively during the course of bulimia nervosa or anorexia nervosa.


Avoidant/Restrictive Food Intake Disorder
A feeding or eating disturbance (e.g. lack of apparent interest in eating food; avoidance based on the sensory characteristics of food; concern about aversive consequences of eating) as manifested by persistent failure to meet appropriate nutritional and/or energy needs associated with one (or more) of the following:
- Significant weight loss (or failure to achieve expected weight gain or faltering growth in children).
- Significant nutritional deficiency.
- Dependence on enteral feeding or oral nutritional supplements.
- Marked interference with psychosocial functioning.
- The disturbance is not better explained by lack of available food or by an associated culturally sanctioned practice.
- The eating disturbance does not occur exclusively during the course of anorexia nervosa or bulimia nervosa, and there is no evidence of a disturbance in the way in which one’s body weight or shape is experienced.
- The eating disturbance is not attributable to a concurrent medical condition or is not better explained by another mental disorder. When the eating disturbance occurs in the context of another condition or disorder, the severity of the eating disturbance exceeds that routinely associated with the condition or disorder and warrants additional clinical attention.
PICA
- Persistent eating of nonnutritive, nonfood substances over the period of at least one month.
- The eating of nonnutritive, nonfood substances the inappropriate to the developmental level of the individual.
- The eating behavior is not part of a culturally supported or socially normative practice.
- If the eating behavior occurs in the context of another mental disorder (e.g. intellectual disability, autism spectrum disorder) or medical condition (e.g. pregnancy), it is sufficiently severe to warrant additional clinical attention.
Individuals with PICA have been reported to mouth and/or ingest a wide variety of nonfood substances, including, but not limited to, clay, dirt, sand, stones, pebbles, hair, feces, lead, laundry starch, vinyl gloves, plastic, pencil erasers, ice, foam rubber, fingernails, paper, paint chips, coal, chalk, wood, plaster, light bulbs, needles, string, cigarette butts, wire, and burnt matches.
Rumination Disorder
- Repeated regurgitation of food over the period of at least one month. Regurgitated food may be re-chewed, re-swallowed, or spat out.
- Not attributable to an associated gastrointestinal or other medical condition (e.g. reflux).
- Does not occur exclusively during the course of anorexia nervosa, bulimia nervosa, binge-eating disorder, or avoidant/restrictive food intake disorder.
- If symptoms occur in the context of another mental disorder (e.g. intellectual disability), they are sufficiently severe to warrant additional clinical attention.
